In previous blog posts, Stillman and Friedland have discussed how treatment can be a double-edged sword. As a patient and as a litigant, what do you need to know? What are some considerations for additional procedures?
On the one hand, expenses for medical treatment are a major determinant of the amount of compensation you are entitled to for your injuries.
On the other hand:
- Outlays for treatment must be proportional to the injuries claimed, and
- More importantly, medical care may be ineffective or detrimental to your health.
- It is up to you to do your homework and make an informed decision.
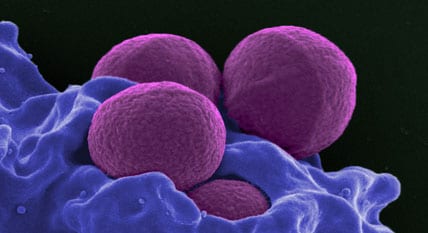
In today’s post, we will look at MRSA infections as a dangerous downside of procedures and hospitalization.
What is MRSA?
The full name is Methicillin-resistant Staphylococcus aureus. The term refers to a “staph” bacterium that has developed a resistance to antibiotic treatment. Generally, it is the intrusion of these fairly common bacteria to soft-tissue injury sites that causes hard-to-control infections. We are used to being able to resolve infections with antibiotics, but in this case, the patient may contract an in-hospital infection which does not respond to antibiotic treatment.
Why does this happen? Many of us grew up in an age when every “bug” was treated by administering antibiotics. Some doctors still practice this way. As many of you know, antibiotics are only useful against bacterial infections. Antibiotics are useless against viruses. Unless the doctor makes certain that your problem is bacterial and not viral (via a lab test), there is no point in just “giving you something”.
Overuse of antibiotics has killed off swathes of bacteria which cannot resist antibiotics, while leaving a population of stronger “super-bugs”. These resistant strains have come to dominate the micro-environment in a number of situations. Often, surgery or repeated surgeries may be required to remove infected tissues.
Here are several versions of this problem:
- CA-MRSA: Community-associated MRSA. This version is a problem in a number of environments, including professional and school sports, and summer camps. Avoid sharing equipment to reduce spreading infection. Washing cuts or scrapes is important, too.
- LA-MRSA: Livestock-associated MRSA. Spread by contact with farm animals or airborne.
- HA-MRSA: Healthcare-associated or Hospital-acquired MSRA. Proliferates in hospital and clinic settings where patients are susceptible and use of antibiotics is widespread.
The underlining commonality in all these MRSA variants is the overuse of antibiotics, creating an environment where super-bugs proliferate. The CA type is associated with close quarters and poor hygiene. When working parents feel pressured to “do something” for their kids to keep them in school or daycare, they may medicate their children (and even themselves) with antibiotics—just in case. This overuse of antibiotics has the reverse of the desired effect—it increases the population of more harmful bacteria. In school and camps where skin and soft tissue injuries (SSTIs) are common, scrapes and cuts may easily develop into MRSA infections. Similarly, in livestock farming, antibiotics are used as a feed additive to spur growth and keep down the infections which can develop in overcrowded feedlots. These feedlots can be MRSA breeding grounds.
If you are a hospital patient you have minimal choices regarding how you are treated and little control over your exposure to MRSA. While these bacteria are a common feature of our bacterial environment, the use of I.V. drips, ports, surgical incisions, surgical intubation, and other skin breaks and invasive procedures leave the patient vulnerable. While hospitals have clear guidelines for good hygienic procedure, realistically, compliance is never going to be 100%. The human factor and accidental contact mean that, even with the best of intent, there is no such thing as total avoidance.
Who Is At Risk?
- Patients in hospital settings who undergo invasive procedures have a higher risk of exposure.
- Individuals with already compromised health are at additional risk.
- Individuals in close quarters such as summer camp, locker rooms and contact sports, and who may share equipment such as helmets and pads, swim flippers, etc. have greater exposure.
- A recent study indicates that among dialysis patients, black patients are at a higher risk for MRSA than white patients. Jumping to socio-economic causes may be poor judgment; association is not causation. Certainly black males suffer higher rates of type II diabetes than the general population, and there may be a link with severity and susceptibility which was not explored. (This was certainly the case for breast cancer fatalities in black women, which were dismissed as solely due to poor care, but instead were caused by an aggressive strain of tumors in younger women. Failure to address the true causes meant failed screening policies and treatment.)
- Canadians: A number of effective anti-MRSA drugs are unavailable under the Canadian health care system as of 2017.
- Those who are overexposed to antibiotics.
How Can You Avoid Exposure?
Infographic Source: CDC
- If you are hospitalized, having someone with you to remind health care workers—tactfully—to follow hygienic procedures can be helpful.
- Avoid “routine” antibiotics unless needed. In this way you can preserve the diversity of bacteria in and on your body.
- Avoid unnecessary procedures. Assess the risk of additional procedures versus the rate of success and improvement. Do your homework to find out the efficacy of the procedure offered. One very large study of back surgeries showed that 70% of patients ended up taking 40% more pain meds post-surgery. A few extra dollars in your settlement will be of little comfort if you develop more chronic pain.
- Treat cuts and scrapes immediately whether they happen in crowded facilities or outdoors.
- Stay in good shape! Healthier patients have fewer complications. Eat a good diet and keep moving.
Because we care…